BC Centre on Substance Use
By Mona Kwong, Pharmacy Advisor and Director, Interdisciplinary Clinical Addiction Fellowship Program — Pharmacy Stream and
Kevin Hollett, Director, Communications and Community Engagement
A renewed call for pharmacists to help end overdose deaths with a focus on stigma-free care and awareness of the latest clinical guidelines and resources
International Overdose Awareness Day occurs on Aug. 31 each year and is the world’s largest annual campaign to end overdose, remember without stigma those who have died and acknowledge the grief of the family and friends left behind. For pharmacists, it is a reminder of the vital role they play in helping prevent toxic drug overdoses in their communities.
The urgent need to prevent overdose deaths has also been recognized as a global issue by the United Nations. Their 2030 Agenda for Sustainable Development — a plan of action for people, planet and prosperity that all countries are expected to implement — reflects the importance of continued action to end toxic drug overdoses as part of the Sustainable Development Goal to Ensure Healthy Lives and Promote Well-Being for All which includes a target to strengthen the prevention and treatment of substance use.
Together we can is the 2024 theme for International Overdose Awareness Day and urges everyone to lean into the power that we can have when we work together. Pharmacists are leaning in, using their knowledge, skills, and abilities and working together with other health-care providers, harm reduction workers, and people who use drugs to help prevent overdose deaths. This work is impactful and needs to continue.
The overdose crisis continues to claim the lives of seven British Columbians and more than 20 Canadians every single day. Unregulated drug toxicity deaths accounts for more deaths than homicides, suicides, accidents and natural disease combined.
Stigma around substance use also contributes to the risk of overdose death through perpetuating assumptions about who is most at risk and the use of harmful language which can create barriers to accessing care.
The 2024 data from the BC Coroners Service revealed that while 71 per cent of those dying from unregulated drug toxicity were male, the death rate for females has nearly doubled since 2020, from about 13, to 23 per 100,000 in 2024. In addition, the greatest proportion of deaths (48 per cent) occurred in private residences, with 35 per cent in other inside residences including social/supportive housing, shelters, and hotels and 16 per cent outside in vehicles, sidewalks, streets or parks.
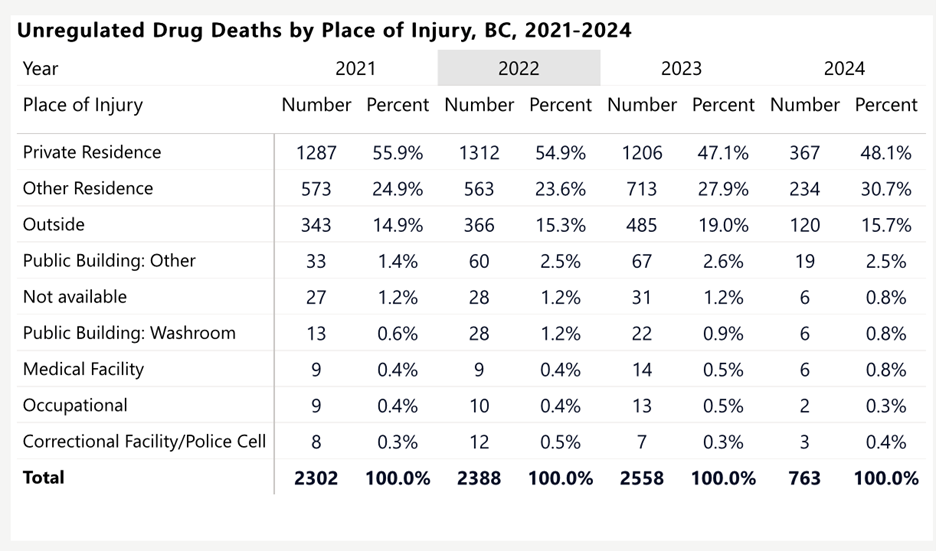
Unregulated Drug Deaths by Place of Injury, BC 2021-2024
Source: BC Coroners Service

Sex-Specific Unregulated Drug Death Rates per 1000,000, 2014-2024
Source: BC Coroners Service
Looking Forward
While the toxic unregulated drug supply is the key driver of fatalities, challenges with accessing comprehensive, evidence-based addiction treatment and care is a major contributor to reducing substance use related harms. A whole system approach is needed to support people who use substances. Pharmacists and pharmacy teams will continue to play a vital role in preventing overdose deaths and need to ensure they are focused on providing stigma-free care and following the latest clinical guidelines.
Both the application of clinical knowledge and the trust built through pharmacist-client relationships provide valuable opportunities for overdose prevention. That’s why it’s important for pharmacists to be aware of the most recent updates to B.C.’s Clinical Guideline for Treating Opioid Use Disorder released in November 2023 and follow best practices for providing stigma-free, culturally safe care.
Pharmacists are one of the most accessible and trusted health care providers in our health care system. This provides the opportunity for pharmacists to play a key role in preventing toxic drug overdoses, working as part of the health-care team to help more people access and experience success with substance use treatment. Together we can means pharmacy teams are an instrumental part of the health-care team and the community in helping change the course of the overdose crisis. Together, we can help build a better and safer system for substance use care.
Using the Latest Guidance to Provide the Best Possible Care
There is now a significant amount of evidence-based information and resources available on the prevention of toxic drug overdoses and the treatment of substance use – pharmacists need to make use of these resources so they are well equipped for crucial conversations with their clients around substance use and supported in their clinical decisions.
Finding Success Through Stigma-Free Care
Pharmacists play an important role in the healthcare team through frequent trust-building conversations and check-ins with clients about their health and wellbeing. As a result, the language used during conversations about substance use is crucial to earning and maintaining trust and helping clients experience success with substance use treatment.
Pharmacists need to aware of and actively work to reduce the stigma experienced by individuals with opioid use disorder, including awareness of the language they use in clinical encounters and its potential to stigmatize individuals who use opioids and other substances.
Pharmacy teams involved in substance use care should strive at all times to use “person-first” language and current medical terminology (eg. person with an opioid use disorder) when interacting with clients, families, colleagues, and other health care professionals, and staff.
It’s important to use the resources available on how stigma impacts substance use treatment and how to use person-first language, including:
- Substance Use Stigma – BC Centre on Substance Use
- Respectful Language and Stigma Regarding People Who Use Substances – BC Centre for Disease Control
- Addressing Opioid Stigma in Pharmacies - CAMH
The latest Guideline for the Clinical Management of Opioid Use Disorder from the BC Centre on Substance Use now also includes specific principles of care related to client-centred care, social determinants of health, cultural safety and humility, anti-racist practices in substance use care, trauma-and violence-informed practice, recovery and self-defined wellness, harm reduction, integrated continuum of care, and self-defined and wellness oriented care.
The BC Centre on Substance Use (BCCSU) is a provincially networked resource with a mandate to develop, implement and evaluate evidence-three strategic areas including research and evaluation, education and training, and clinical care guidance.
Both its updated Guideline for the Clinical Management of Opioid Use Disorder and many other resources – including a 24/7 Addiction Medicine Clinician Support Line – are valuable for pharmacists involved in providing substance use treatment.
Opioid Agonist Treatment Compliance And Management Program For Pharmacy
OAT CAMPP training has undergone a major update to be aligned with these clinical and regulatory changes and can be found in the BCPhA eTraining Portal (bcpharmacy.ca/etraining). For more information, see the BCPhA OAT CAMPP registration page bcpharmacy.ca/OAT.
Updated Guideline for the Clinical Management of Opioid Use Disorder
In November 2023, a second edition of the Guideline for the Clinical Management of Opioid Use Disorder was released by the BCCSU to ensure that health care providers have access to updated clinical guidance aligned with the best available evidence on interventions across the continuum of opioid use disorder care.
Key changes include:
- Addition of principles of care including client-centred care, social determinants of health, cultural safety and humility, anti-racist practices, trauma-and violence-informed practice, recovery and self-defined wellness, harm reduction, integrated continuum of care, comprehensive health management, and self-defined and wellness-oriented care.
- Shifting away from first/second/third line treatments to specific client circumstance, goals and previous treatment experience. Buprenorphine/naloxone is no longer suggested as a first line treatment followed by methadone and slow-release oral morphine.
- Addition of a long-acting injectable buprenorphine option which may be offered to those stabilized on buprenorphine/naloxone
- Alignment with CRISM iOAT Guidelines with the addition of injectable OAT with diacetylmorphine or hydromorphone to be considered for those adults with severe OUD and unregulated injection opioid use who have not benefitted from or have declined oral options for OAT
- OAT dosing, titration, missed doses, dosing protocols, and take-home dosing have changed
- Addition of a Continuing Care Appendix
- Guidance on buprenorphine/naloxone initiation in emergency room departments
- Updated guidance on urine drug testing
Additional Resources From the BC Centre on Substance Use
In addition to the Guideline for the Clinical Management of Opioid Use Disorder, the BCCSU has a variety of resources available to support healthcare providers involved in providing substance use treatment, including a 24/7 Addiction Medicine Clinician Support Line that pharmacist can use.
Key resources include:
- Provincial Opioid Addiction Treatment Program
- Addiction Care and Treatment Online Certificate
- BC ECHO on Substance Use
- Interdisciplinary Clinical Addiction Fellowship Program (Largest program in North America for Medicine, Nursing (NP/RPN), Pharmacy Social Work)
- Clinical Resources for Opioid Use Disorder
- Practical Administration of Sublocade Injection
- Canadian Clinical Guideline High-Risk Drinking and Alcohol Use Disorder
Addiction Medicine Clinician Support Line
The 24/7 Addiction Medicine Clinician Support Line provides telephone consultation to physicians, nurse practitioners, nurses, midwives, and pharmacists who are involved in addiction and substance use care and treatment in British Columbia. The Support Line connects health care providers to an Addiction Medicine Specialist who has expertise and knowledge in addiction medicine (including emergency, acute, and community care). Consultation can include support in screening, assessment, treatment and management of substance use and substance use disorder(s). In partnership with FNHA, the line also supports Indigenous communities in BC to access to addiction consult phone services. This service extends beyond clinicians and provides addiction medicine guidance to any addiction support staff calling from Indigenous communities within B.C., including Indigenous urban centres.

