The BC Pharmacy Association is advocating for more support for rural communities. Rural health care needs our help. Here are eight recommendations that will help pharmacies deliver better health care in rural and remote British Columbian communities.
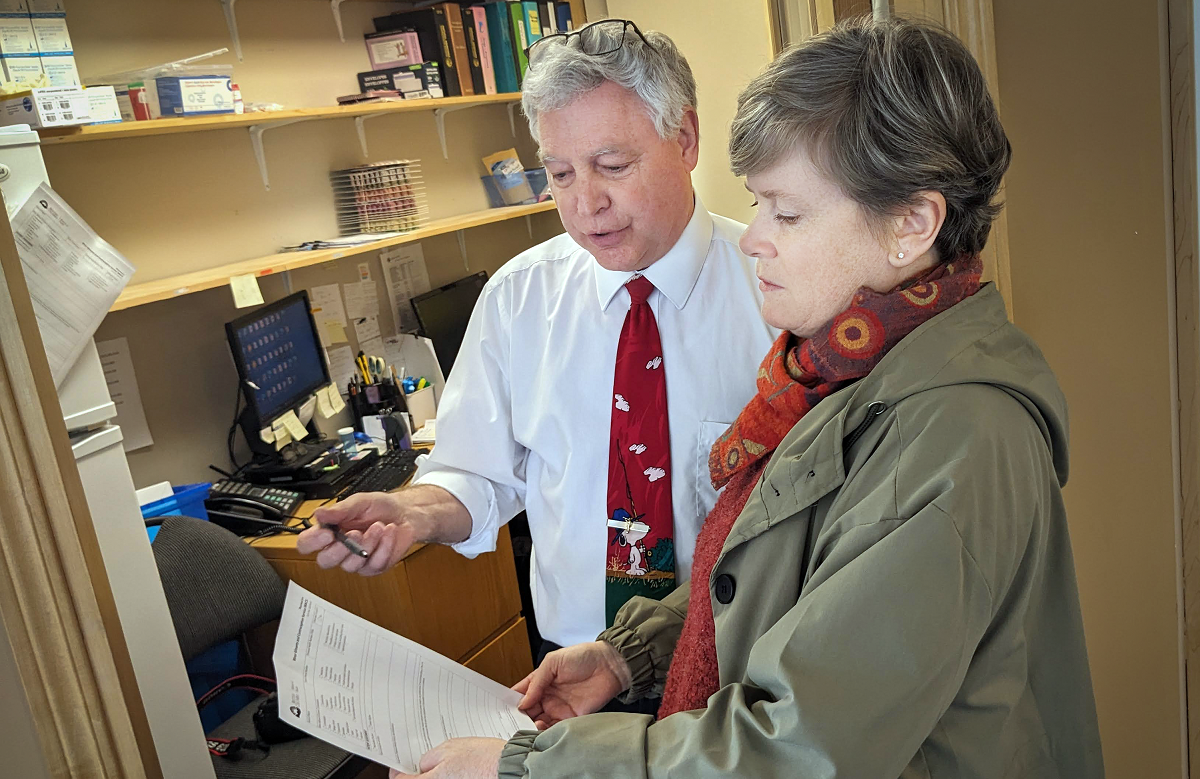
Larry Johannessen, owner of Medicine Shoppe #253, speaks with MLA Josie Osborne, Minister of Energy and Mines for B.C., about the importance of rural pharmacies to communities like Port Alberni.
By Michael Mui
Communications Manager, BCPhA
After more than 30 years, pharmacist Larry Johannessen is thinking about hanging up his white coat. At 69 years old, the former semi-truck driver, road paver, logger and pastor has had a full life. His children are grown, and one of them has even chosen to follow in his footsteps, obtaining a Doctor of Pharmacy degree in 2020.
Johannessen grew up in Port Alberni, a central-Vancouver Island city that’s home to just under 20,000 residents. Over the course of his career, he owned and operated three of the 10 pharmacies in the community. Initially, he had the intention of passing the operation of his pharmacies to his pharmacist son, but of late, those plans are changing.
“The cost of living here in British Columbia is just too much. My son is the sole breadwinner in his family and he’s looking south to the United States because there’s better earning potential and the cost of housing is cheaper,” Johannessen said. “He was operating one of my pharmacies, but he left last July and I had to close the store. If I can’t find a replacement manager for another of my stores this year, it too will have to close.”
Johannessen’s story is similar to the stories of many British Columbian pharmacists who work in remote communities. Many say they have difficulties attracting and retaining staff, are working long hours at their own expense, and must constantly advertise a premium to attract the few pharmacists that are interested in working in remote communities. And quite often, even when a pharmacist can be convinced to work outside of the big city, many don’t stay long.

Janette Bowering, pharmacy manager at Save-on-Foods Pharmacy #2214, speaks with MLA Roly Russell about the types of supports pharmacies like hers could benefit from.
A lack of pharmacists in rural areas
Janette Bowering, pharmacy manager at Save-on-Foods in Grand Forks, has seen her pharmacy downsize from three pharmacists to just one, all in the space of a few years. With only one pharmacist at her location, her company has had to reduce the number of hours her pharmacy is open for. The only way she receives any time off is when a relief pharmacist is flown in from out of town.
“Many pharmacists would rather work in an area closer to the city or where their family and friends are. It’s hard to attract people to come out to Grand Forks, and even when there is someone interested, our housing supply is limited and costs are not that much cheaper than they are in the city,” Bowering said.
In October 2023, the BC Pharmacy Association struck a Rural Pharmacy Working Group to identify critical challenges pharmacists in rural communities are facing, with the aim of identifying recommendations that could mitigate concerns.
The Association heard that challenges include, but are not limited to, workforce shortages, difficulty in recruiting and retaining pharmacists and staff, lack of locum and relief support, lack of digital infrastructure, shortage of housing, and no formal support system for new graduates or out-of-province pharmacists considering rural practice.
The reality is, according to data from the Canadian Institute of Health information, fewer pharmacists are choosing to work in rural areas compared to urban ones. Additionally, new grads are often turning to hospital instead of community pharmacy, or opting to serve in industry or education roles instead.
This lack of adequate staffing in rural communities has placed additional burden on those who continue to serve in these communities, and existing supports, such as B.C.’s Rural Incentive Program — which provides financial supports for a very small number of pharmacies that meet its criteria — are not going far enough.
In spring 2024, these findings along with eight recommendations were presented to the B.C. Ministry of Health.

Aaron Sha, associate owner of Shoppers Drug Mart #2256 in Prince Rupert, poses for a photo at Totem Park in the seaside community.
Rural pharmacies face similar challenges across B.C.
Aaron Sha, associate owner at Shoppers Drug Mart #2256 in Prince Rupert, moved from the Lower Mainland to the northern B.C. community nearly two years ago when the opportunity for an associate owner position came up.
Since then, however, he has been unable to attract new pharmacists despite offering wages significantly higher than what would be considered the norm in larger cities.
The only reason he’s able to staff his pharmacy at all is because his wife is also a pharmacist, and the couple have split their schedules to ensure there’s someone at the pharmacy seven days a week.
“We almost never see each other. When she is at home, I am at work. Once a month, I’ll book a relief pharmacist to come in so we can have a weekend together,” Sha said. “But even that has a significant cost. I have to pay for their flight, their accommodation, and offer much more than what a regular pharmacist would earn per hour.”
Johannessen, Bowering and Sha all recently met with their provincial Members of the Legislative Assembly, politicians who represent their communities, to discuss how government may better support pharmacies in rural areas.
All three agreed that the challenges associated with operating a pharmacy in rural B.C. have grown since the pandemic, for the same reasons as those identified by the Association.
“Lack of pharmacists has definitely impacted service levels. During flu season, we had to ask patients to wait for minor ailments assessments, sometimes in excess of 30 minutes, and many patients left without being seen,” Sha said.

Students of the University of B.C.'s Faculty of Pharmaceutical Sciences participated in a rural pharmacy panel in March to hear from pharmacists practicing in rural areas.
Students’ perspectives on rural B.C.
Despite the difficulties many pharmacies have in attracting new graduates interested in working in B.C.’s remote and rural areas, some students are bucking the trend.
Ilianna Doornbos, a third year PharmD student at UBC, moved from Prince George to Vancouver for school. One of the barriers she sees to encouraging rural residents to take up professions such as pharmacy is the current lack of student loan forgiveness programs for pharmacists.
The current federal Canada Student Loan forgiveness program only provides eligibility for nurses and medical doctors serving in under-served rural or remote communities. That may change soon — with pharmacists being slated for inclusion in the Canada Student Loan program as part of the 2024 federal budget. B.C. also has a student loan forgiveness program, but that program also excludes pharmacists. Doornbos is hoping similar changes will be made to the provincial forgiveness program.
“For students in rural and remote areas, when they think of doing a program like pharmacy, medicine or dentistry, often many of us are told how that program is expensive or competitive because it’s based in Vancouver, and that taking on the program is going to result in substantial debt. Why would you consider such a program when you can go into a trade or work at the mill?” Doornbos said.
“Our tuition is almost as expensive as med school. I had to rely on student loans and was thankfully eligible for a line of credit to pay for the rest of the program. Even so, I had to ask my mom to be a cosigner.”
Doornbos believes incentivizing students who were raised in remote areas of B.C. to become pharmacists will help with the shortage of pharmacists in rural and remote areas. As someone from northern B.C., she has always intended to return to her home region upon graduation.
“Being from rural B.C., I can confidently say that when health-care professionals move to communities like Prince George or Smithers that once they move, they settle down and they start to fall in love with the area,” she said.
“We have a shortage of pharmacists across B.C., regardless of whether you’re in an urban or rural area, but the rural, remote and isolated areas in B.C. are hurting even more than in Vancouver.”
For students, at least, the appeal of rural practice appears to be growing. In February, students at the University of B.C.’s Faculty of Pharmaceutical Sciences approached the BCPhA to host a rural pharmacy panel, inviting pharmacists who practice in rural communities to share their experiences.
Karyssa Boyle, a second year pharmacy student and a BCPhA student ambassador, said they chose the topic because students have limited exposure to rural pharmacy within the existing PharmD program, and the aim was to help provide some insights to those students who may be interested in pursuing a career in rural B.C. in their future.
“Rural communities in B.C. have reduced access to health care and face a variety of health inequities. With our expanding scope of practice and current skill set, pharmacists are well equipped to make a difference in underserved communities as frontline health care providers,” Boyle said.
“We believe our profession can bridge the health-care gap in our province and encourage students to practice where their clinical skills can have a profound impact.”

The semi-rural community of Gibsons, B.C.
Working in rural communities has its rewards
Catherine McCann, owner of Medicine Shoppe #169 in Comox, was one of a few pharmacists invited to speak to UBC students at the rural pharmacy panel. She recalled her first experience as a pharmacist in a small town, it was her first job after graduation.
For her, she believes one challenge new graduates must overcome when working in a rural community is building confidence.
“My first experience out of university, I was thrown in a small, small town practice. The owner handed me the keys and went on vacation. Talk about being thrown on the deep end, right?” McCann said.
“You might experience some failures but this is how you learn. What I hoped the students would take away is that rural communities have a ton of rewards. I live in a beautiful community. I have really good relationships with all of my patients. You get to build a community here and you get to do some pretty good work here as a clinician.
“Despite all of the challenges there are some beautiful things you can do in a rural community.”
Atsushi Sato, pharmacy manager at London Drugs in Gibsons, was another pharmacist who was invited to speak at the students’ rural panel. After graduating from pharmacy school in Japan, he became certified to practice as a pharmacist in Canada. Since then, he’s spent the last 16 years practicing in Gibsons.
There have been many changes in recent years in the staffing situation and workload of pharmacists, he said, including how competitors started paying high wages to attract pharmacists to keep their pharmacy operations running.
Wages are definitely one of the biggest factors but there are not many pharmacists who choose to settle here for the long term,” Sato said.
As a newly licenced international graduate with no ties to B.C.’s urban areas, the decision to practice outside of the city was an easy one.
“I work a lot of overtime but also have control to maintain a good work-life balance,” Sato said, adding that he likes the family-friendly lifestyle that a semi-rural area affords, a factor that is echoed almost universally by his colleagues who also work outside of the city.
None of the pharmacists and pharmacies featured in this article currently qualify for rural subsidies from the provincial government, as all the pharmacies do not meet the criteria of being the only pharmacy in their communities, with the next closest pharmacy at least 25 kilometres away or requiring a ferry ride to reach, along with having a relatively low script count.
“I think the most important piece is that definition of what is rural,” said McCann. “If they looked at where I practiced right now, they’d say I’m not rural because there are a good number of pharmacies in the Comox Valley area. But that doesn’t change the challenges I face like getting a locum, getting supplies, all of that kind of stuff because I’m far away from a major centre.”
For Johannessen, the pharmacist in Port Alberni, he’s hoping that one day the situation would improve again to a point when he will be able to hire enough staff to consider retirement. He’d like to retire soon, but then his patients would have nowhere to go.
“My first and foremost concern is my patients. We need people who are willing to be pharmacy managers. Not just pharmacy managers, but also pharmacists, pharmacy technicians and pharmacy assistants. If we could get them to come, that would be super,” he said.
“It was only 10 or 15 years ago when we actually had staff.”

The above is an advertisement. For more information please contact michael.mui@bcpharmacy.ca
