By Jane Xia, BSc.Pharm, PharmD, MBA, RPh
This article was funded by Organon Canada which had the opportunity to review and comment
Can Pharmacists in British Columbia Prescribe Long-Acting Reversible Contraceptives (LARCs)? Absolutely! Pharmacists in British Columbia are permitted to prescribe Long-Acting Reversible Contraception (LARC) such as intrauterine devices (IUD) according to the Health Professions Act – Pharmacists Regulation1,2.
While pharmacists are authorized to prescribe LARCs, we acknowledge that there are still notable challenges along the patient journey, particularly because pharmacists currently cannot perform insertions for IUDs or implants. Such limitations pose significant obstacles for community pharmacies in delivering comprehensive contraceptive care, especially to patients suited for LARCs.
Before exploring these challenges and potential solutions, let’s review the available LARCs in Canada and some key counselling points for patient interactions.
Overview of LARCs
Unintended pregnancy is a common issue in Canada. Nearly 50% of all pregnancies in Canada are unplanned. This can be a difficult experience for women of all ages, from adolescence to near menopause9. IUDs and contraceptive implants, collectively known as LARCs, are over 99% effective in preventing unwanted pregnancies3. Despite their efficacy, LARC methods have not been regularly presented or discussed with women regarding contraception due to barriers such as limited knowledge4 and cost8. However, with all contraceptive methods now covered under BC Pharmacare, the cost barrier has been significantly reduced, allowing women greater autonomy in selecting these options.
Society of Obstetricians and Gynaecologists of Canada (SOGC) suggests that one way to approach the conversations when discussing the different types of contraceptive methods is to inquire about the desire for pregnancy. This will help focus the discussion on either LARC or Short-Acting Reversible Contraceptives (SARC). SOGC has adapted Dr. Rupinder Toor’s decision tree11:
- When do you want to be pregnant, if ever?
- How important is it for you NOT to be pregnant until then?
If the patient indicates that avoiding pregnancy is very important for at least one year or indefinitely, LARC options should be discussed. LARCs are available in both hormonal and non-hormonal options.
For hormonal options, there is a subdermal implant, etonogestrel 68 mg13, which is placed just under the skin on the inner side of the non-dominant upper arm. Additionally, there are intrauterine devices (IUDs) containing either 52 mg or 19.5 mg of levonorgestrel, designed for vaginal insertion14,15. All are indicated for conception control.
For those seeking non-hormonal LARC options, copper IUDs come in various concentrations, allowing for customization based on desired duration of protection (5-10 years) and suitability based on uterine size and/or parity.

See references 13, 14 and 15.
Prescribing LARCs and Community Pharmacy Practice
Community pharmacy practice faces several general limitations, such as space, time, and language barriers. When it comes to LARC prescribing, one of the biggest challenges is that we cannot provide the insertion service ourselves. Furthermore, we are often not connected to a physician clinic that can offer this service promptly. Worse yet, there is a concern that the prescribed LARC may not be accepted by the health care provider performing the insertion, leading to wasted system resources and patient time.
So, how can we better serve patients who are ideal candidates for LARCs, even though we cannot currently provide the insertion service at the pharmacy? Here are some ideas and suggestions to help streamline the process of providing LARC services at the pharmacy.
Build Local Relationships Before Prescribing:
Establishing a strong network is essential for pharmacists providing LARCs, as we cannot perform insertions ourselves. Whether working in an independent pharmacy or a large corporate chain, pharmacists must take the lead in guiding patients on where to go, what to expect, and how to access services to ensure a seamless patient journey. Partnering with trained professionals, such as physicians, nurse practitioners, midwives, or naturopathic doctors for LARC insertions is crucial for creating a clear pathway for patients. Especially with wait times for appointments, you may need to troubleshoot and consider providing a SARC until the patient is able to secure a LARC insertion appointment. Building a network of key providers enhances the patient experience by offering valuable insights into the process.
To ensure accurate and up-to-date information regarding the insertion of LARCs by different health professionals before establishing a partnership, consider consulting the regulatory college of the profession in the applicable province/territory.
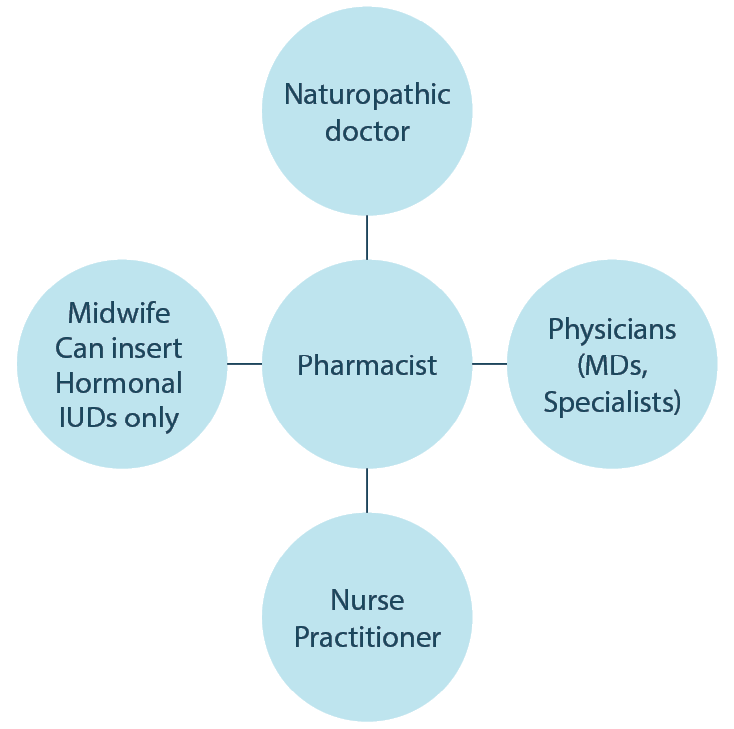
Note: Midwives are authorized to insert hormonal IUDs but not copper IUDs. It’s crucial to understand the scope of practice for your health care partners.
Leverage Corporate Support for Streamlined Setup
If you work in a corporate pharmacy and prescribing LARCs aligns with your pharmacy’s goals, consider leveraging corporate support to streamline the setup process and enhance the patient experience. Head offices can help establish a clear pathway for patients, which may include hiring a nurse practitioner for clinic days to insert IUDs or implants at locations with suitable space or private consultation rooms. Additionally, established connections with pharmaceutical representatives can provide resources regarding insertions and offer details on wait times. This centralized approach helps create a smoother experience for patients while improving access to essential services.
Train Staff to Enhance Patient Experience
No matter which pharmacy you work for, it is essential to train pharmacy staff to understand the patient journey. This ensures that when a patient asks questions, staff are well-informed and not left unsure of how to respond. Staff should be able to clearly articulate the process or provide a general but reassuring response, demonstrating that the pharmacy is equipped to offer all contraceptive options by prescription. For LARCs, they should convey that patients can expect a straightforward and seamless experience.
While there are still challenges in providing LARCs in community pharmacies, pharmacists can take proactive steps to improve patient care. By building local relationships, leveraging corporate support, and training staff, pharmacists can enhance the patient journey related to LARCs options. By working collaboratively with health care providers, pharmacists can help empower patients to make informed choices and access contraceptive care.
Note: IUS is used interchangeably with IUD in this article.
- British Columbia Pharmacy Association. FAQs for Pharmacists on Minor Ailments and Contraception Services. 21 Oct. 2024. Accessed 19 Nov. 2024.
- BC Law. BC Health Professions Act – Pharmacists Regulation. 1 June 2023. Accessed 10 Jan. 2025.
- Stark, Elizabeth L., Amanda M. Gariepy, and Myra Son. “What Is Long-Acting Reversible Contraception?” JAMA, vol. 328, no. 13, 2022, p. 1362. doi:10.1001/jama.2022.14239.
- Kaye, Kristin, Catherine Suellentrop, and Corinna Sloup. The Fog Zone: How Misperceptions, Magical Thinking, and Ambivalence Put Young Adults at Risk for Unplanned Pregnancy. National Campaign to Prevent Teen and Unplanned Pregnancy, 2009.
- Tang, Jessica, Robin Maurer, and Deborah Bartz. “Intrauterine Device Knowledge and Practices: A National Survey of Obstetrics and Gynecology Residents.” Southern Medical Journal, vol. 106, no. 9, 2013, pp. 500–505. doi:10.1097/SMJ.0b013e3182a5ef0a.
- Harper, Cynthia C., et al. “Evidence-Based IUD Practice: Family Physicians and Obstetrician-Gynecologists.” Family Medicine, vol. 44, no. 9, 2012, pp. 637–645.
- Harper, Cynthia C., et al. “Counseling and Provision of Long-Acting Reversible Contraception in the US: National Survey of Nurse Practitioners.” Preventive Medicine, vol. 57, no. 6, 2013, pp. 883–888. doi:10.1016/j.ypmed.2013.10.005.
- Universal Access to No-Cost Contraception for Youth in Canada. Canadian Pediatric Society. Accessed 10 Jan. 2025.
- The Society of Obstetricians and Gynaecologists of Canada. PregnancyInfo: Unintended Pregnancy. Accessed 10 Jan. 2025.
- Coffey, M. “LNG-IUS (Mirena) IUD for Emergency Contraception.” This Changed My Practice by UBC CPD. Accessed 2 Jan. 2025.
- The Society of Obstetricians and Gynaecologists of Canada. Counselling for Contraception Guide. APIL. Accessed 2 Jan. 2025.
- Kavanaugh, Megan L., et al. “Long-Acting Reversible Contraception for Adolescents and Young Adults: Patient and Provider Perspectives.” Journal of Pediatric and Adolescent Gynecology, vol. 26, no. 2, 2013, pp. 86–95. doi:10.1016/j.jpag.2012.10.006. Epub 31 Dec. 2012. PMID: 23287602; PMCID: PMC3672067. Accessed 10 Jan. 2025.
- Organon. Etonogestrel (Implanon) Product Monograph. Accessed 2 Jan. 2025.
- Bayer. Mirena Product Monograph. Accessed 2 Jan. 2025.
- Bayer. Kyleena Product Monograph. Accessed 2 Jan. 2025.
- Ali, Moazzam, et al. “Extended Use Up to 5 Years of the Etonogestrel-Releasing Subdermal Contraceptive Implant: Comparison to Levonorgestrel-Releasing Subdermal Implant.” Human Reproduction, vol. 31, no. 11, 2016, pp. 2491–2498. doi:10.1093/humrep/dew222.
- Nurse Practitioners. HealthLink BC. Accessed 10 Jan. 2025.
- BCCNM. Framework for Certification in IUD Contraception Insertion. Accessed 10 Jan. 2025.
- Medsask. Comparison: Copper IUD. Feb. 2023. Accessed 10 Jan. 2025.
